Outcome predictors for Gamma Knife radiosurgery on brain tumors (vestibular schwannoma)
01 october 2015Project description
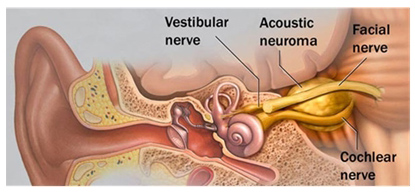
People suffering from unexplained unilateral hearing loss, ringing and buzzing in the ears (tinnitus) or dizziness might have developed a vestibular schwannoma. A vestibular schwannoma, also known as acoustic neuroma or cerebellopontine angle tumor, is a benign, usually slow-growing, primary intracranial tumor that develops from the balance and hearing nerves supplying the inner ear. The tumor arises from the Schwann cells, which are responsible for the myelin sheath surrounding the nerves. As the tumor grows, it presses against the hearing and balance nerves, causing the previously mentioned symptoms. If the tumor progresses further, it might even interfere with the trigeminal nerve, which is the face sensation nerve, causing facial numbness, or the facial nerve, causing facial weakness or paralysis on the side of the tumor. If the tumor becomes large, it will eventually press against nearby brain structures such as the brainstem and cerebellum and becomes life threatening.
This type of tumor is usually diagnosed using magnetic resonance imaging (MRI). After diagnosis three different treatment options are possible: wait-and-scan (or wait-and-see), surgery and radiosurgery. Because treatment of the vestibular schwannoma is done to prevent further tumor progression and does not reduce symptoms, first a wait-and-scan policy is used to determine tumor progression. When the tumor is progressing, the patient is invited for further treatment. Due to the difficult location of this type of tumor, surgery is not preferred. Especially for the patient as this kind of procedure is very invasive and involves hospitalization on intensive care units and a high risk of complications. Radiosurgery is less invasive and is performed in a single day without hospitalization. Also complications are less likely to emerge after treating vestibular schwannoma with radiosurgery.
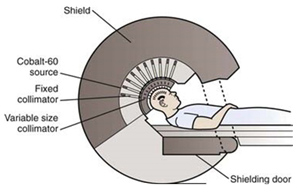
One way of performing radiosurgery is Gamma Knife radiosurgery. This method uses 192 small beams of gamma radiation which are focused simultaneously at a single spot. This enables the delivery of a single, finely focused, high dose of radiation to a target, while causing little to no damage to surrounding tissue. Goal of this treatment is to halt tumor progression by destroying cells and disrupting blood circulation in the tumor. The result of treatment is monitored using MRI. This is done periodically to make sure that the tumor progression is indeed stopped.
 |
 |
In approximately 90% of the cases Gamma Knife radiosurgery succeeds. Tumor progression is stopped and the tumor might even shrink. In the other case, secondary treatment is needed because the tumor progression is not stopped. Why treatment fails is not clear. It might be due to the treatment method or treatment planning, where not all cells are affected enough by the radiation. It might also be due to tumor biology. If treatment success can be predicted, treatment selection can be improved significantly. If a patient is more suited for surgery, he or she can also be better informed as to why this treatment is selected and the overall results of the treatments will increase. This is beneficial for the patient, because he/she will likely only need to undergo one treatment and is better informed about the possible results. It is also beneficial for the follow-up protocol, where predicted tumor progression or shrinkage will lead to a more specific and patient-related follow-up protocol.
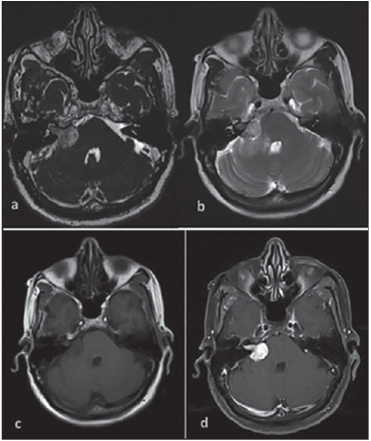
In this study, we retrospectively investigate the MRI series at treatment and attempt to find evidence-based predictive parameters describing the effects of the treatment. For each of these parameters, it can be decided on an individual basis, whether Gamma Knife radiosurgery will be an effective treatment for vestibular schwannoma. Predefined parameters that will be analyzed, both quantitatively and qualitatively, are tumor morphology, heterogeneity, volume, contrast enhancement patterns and density. These parameters reflect the properties of the tumors on the image and will be translated into digital descriptors. Extensive image analysis algorithms will be applied to define these digital descriptors and statistical learning and correlation techniques will be exploited for determining the predictive image features in combination with the clinical data.
This project is a cooperation by Stichting Elisabeth-TweeSteden Ziekenhuis Tilburg, Radboud UMC Nijmegen and Eindhoven University of Technology. Key researchers are Ir. Patrick Langenhuizen, Dr. Jeroen Verheul (MD), Dr. Sveta Zinger and Prof.dr. Peter H.N. de With.
In approximately 90% of the cases Gamma Knife radiosurgery succeeds. Tumor progression is stopped and the tumor might even shrink. In the other case, secondary treatment is needed because the tumor progression is not stopped. Why treatment fails is not clear. It might be due to the treatment method or treatment planning, where not all cells are affected enough by the radiation. It might also be due to tumor biology. If treatment success can be predicted, treatment selection can be improved significantly. If a patient is more suited for surgery, he or she can also be better informed as to why this treatment is selected and the overall results of the treatments will increase. This is beneficial for the patient, because he/she will likely only need to undergo one treatment and is better informed about the possible results. It is also beneficial for the follow-up protocol, where predicted tumor progression or shrinkage will lead to a more specific and patient-related follow-up protocol.
Partners


